Reference-Based Pricing:
A Mid-Market Game-Changer
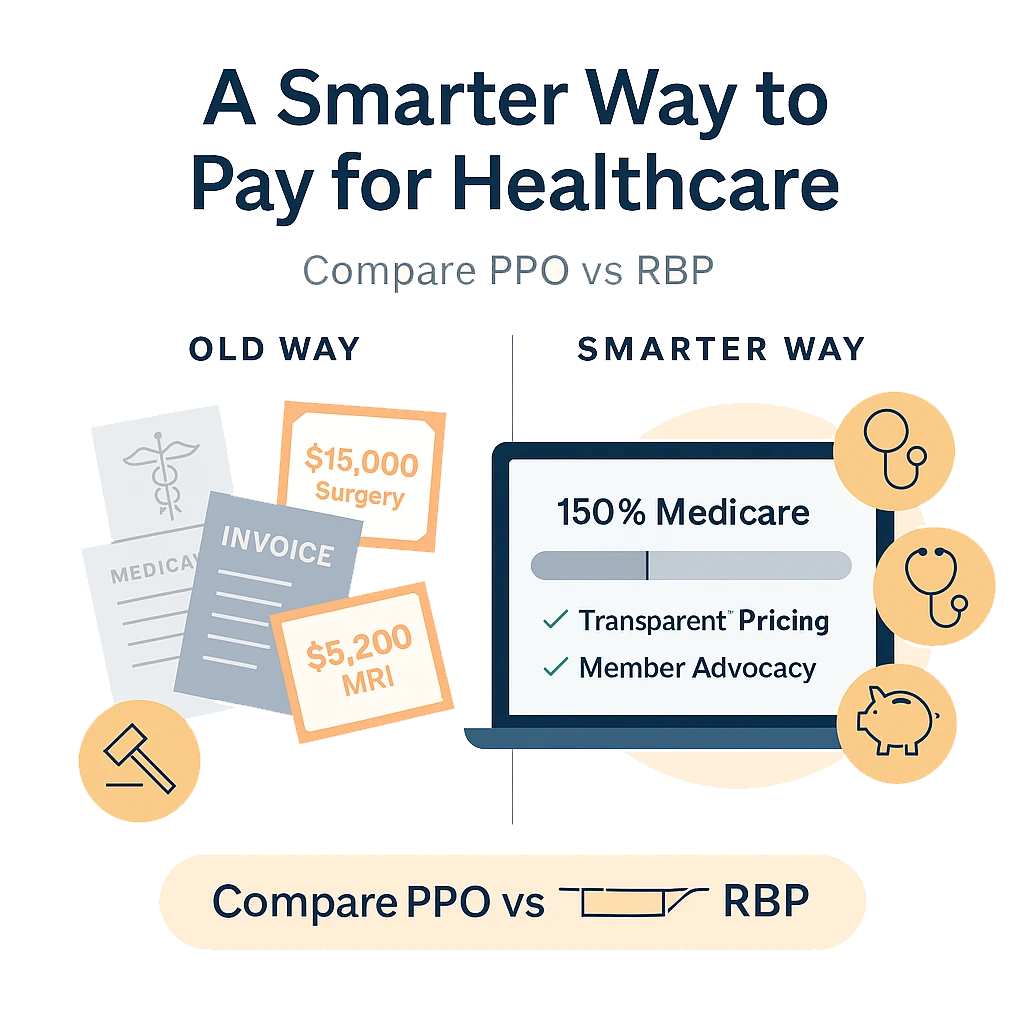
Rising healthcare costs are hitting mid-market companies hard. While traditional PPO networks promise broad provider access, they often deliver the opposite—limited transparency and escalating premiums that can derail your budget. For employers managing 50-500 employees, there's a smarter alternative worth exploring: Reference-Based Pricing (RBP).This comprehensive guide breaks down everything you need to know about RBP, from how it works to whether it's the right fit for your workforce. You'll discover real-world cost savings potential and learn what legal considerations matter most when making this strategic shift.
What is Reference-Based Pricing?
Reference-Based Pricing represents a fundamental shift from traditional healthcare payment models. Instead of accepting pre-negotiated PPOrates that vary wildly between providers, RBP establishes a clear benchmark—or reference point—for what your plan will pay for specific medical services.Here's how it works: Your plan sets payment amounts based on objective criteria like Medicare rates (often 140-200% of Medicare) or regional averages. When an employee receives care, the plan pays the predetermined amount directly to the provider. This approach eliminates the mystery pricing that plagues traditional networks.
The Traditional PPO Problem
Most employers don't realize how PPO contracts actually function. Insurance carriers negotiate different rates with each provider, creating a complex web of pricing that lacks transparency. A simple MRI might cost $500 at one facility and $3,000 at another—both within the same network.PPO plans also limit your control over healthcare spending. You're essentially buying a black box where carriers determine pricing, provider relationships, and ultimately, your renewal rates.
RBP vs. PPO Networks: The Real Comparison
Advantages of Reference-Based Pricing
Cost Predictability: RBP delivers transparent pricing from day one. You know exactly what your plan will pay for each service, making budget forecasting significantly more accurate.
Direct Savings: Companies typically see 20-40% reduction in healthcare costs during the first year. These savings compound over time as you avoid the annual premium increases common with traditional plans.
Provider Choice: Unlike restrictive PPO networks, RBP allows employees to visit any provider.This expanded access often means shorter wait times and better care options.
Claims Transparency: Every claim payment ties back to your established reference point, providing clear insight into healthcare spending patterns.
PPO Network Limitations
Hidden Pricing: PPO contracts obscure actual costs, making strategic planning nearly impossible.
Limited Negotiation Power: As a mid-market employer, you have minimal influence over PPO rate negotiations.
Annual Increases: PPO premiums typically rise 8-15% annually, regardless of your claims experience.
Network Restrictions: Employees face limited provider choices, potentially compromising care quality.
Legal Considerations and Member Advocacy
Implementing RBP requires careful attention to legal compliance and employee communication. The key lies in robust member advocacy support.
Essential Legal Framework
Your RBP strategy must include comprehensive member advocacy services. When providers bill above your reference amount, your advocacy team negotiates on behalf of employees. This protection ensures members aren't caught in billing disputes.
ERISA Compliance: RBP plans must meet all ERISA requirements, including proper plan documentation and fiduciary responsibilities.
State Regulations: Some states have balance billing protections that complement RBP strategies, while others require additional member safeguards.
Documentation Requirements: Clear plan language explaining RBP methodology protects both employer and employees from potential disputes.
Member Advocacy in Action
Professional advocacy teams handle provider negotiations, claims disputes, and member questions. Employees receive dedicated support throughout the healthcare experience, often resulting in better outcomes than traditional PPO customer service.
Real-World Cost Savings Analysis
The financial impact of RBP becomes clear when comparingactual claims data. Here are two key metrics that demonstrate RBP effectiveness:
Average Cost Per Service Comparison
Traditional PPO plans show wide variation in costs for identical services. A knee replacement might range from $15,000 to $45,000 within the same network. RBP establishes consistent pricing—for example, 150% of Medicare rates—creating predictable costs regardless of provider choice.
Annual Healthcare Spend Trends
Companies using RBP typically experience:
Year 1: 20-30% cost reduction compared to previous PPO spending
Year 2-3: Continued savings of 15-25% below market trends
Long-term: Sustainable cost management with annual increases of 3-5% versus PPO increases of 8-15% These savings allow employers to reinvest in employee benefits, expand coverage options, or improve their competitive position in talent acquisition.
Is RBP Right for Your Workforce?
Determining RBP suitability requires honest assessment of your company culture and employee demographics.
Ideal RBP Candidates
Cost-Conscious Organizations: Companies prioritizing healthcare cost management while maintaining quality care access.
Flexible Workforces: Employees who value choice and are comfortable advocating for themselves with provider support.
Growing Companies: Organizations seeking sustainable healthcare cost structures that won't derail expansion plans.
Technology-ForwardTeams: Workforces comfortable using digital tools for healthcare navigation and cost transparency.
Potential Challenges
Change Management: Some employees prefer familiar PPO structures, requiring clear communication about RBP benefits.
Geographic Considerations: Rural areas with limited provider options may present networking challenges.
High-MaintenanceClaims: Employees with complex medical conditions might initially require more advocacy support.
Making the Decision
Consider these factors when evaluating RBP:
Current healthcare costs trending above industry averages
Employee demographics skewing toward educated, tech-savvy workers
Leadership commitment to transparent healthcare cost management
Willingness to invest in proper member advocacy and communication
Ready to Explore RBP for Your Organization?
Reference-Based Pricing offers mid-market companies a powerful tool for controlling healthcare costs while expanding employee choice.The key to success lies in partnering with experienced administrators who understand both the opportunities and challenges of RBP implementation.At Fox Everett, we specialize in helping companies navigate the transition to Reference-Based Pricing. Our boutique approach ensures personalized support throughout the process, from initial evaluation to ongoing member advocacy.
Request a Network Strategy Review
Discover how RBP could transform your healthcare cost structure. Our team will analyze your current spending, assess workforce suitability, and provide a clear roadmap for potential savings.The penalty of excellence means choosing solutions that deliver superior results, even when they require stepping beyond traditional approaches. RBP might be that solution for your organization.


