ACA Reporting Changes in 2025: Are You Ready?
The IRS isn't playing games with ACA compliance anymore. New reporting requirements, tighter deadlines, and state-specific mandates are reshaping how employers handle 2025 ACA filings. Smart companies prepare now—because penalties hit harder than ever when you're caught off guard.
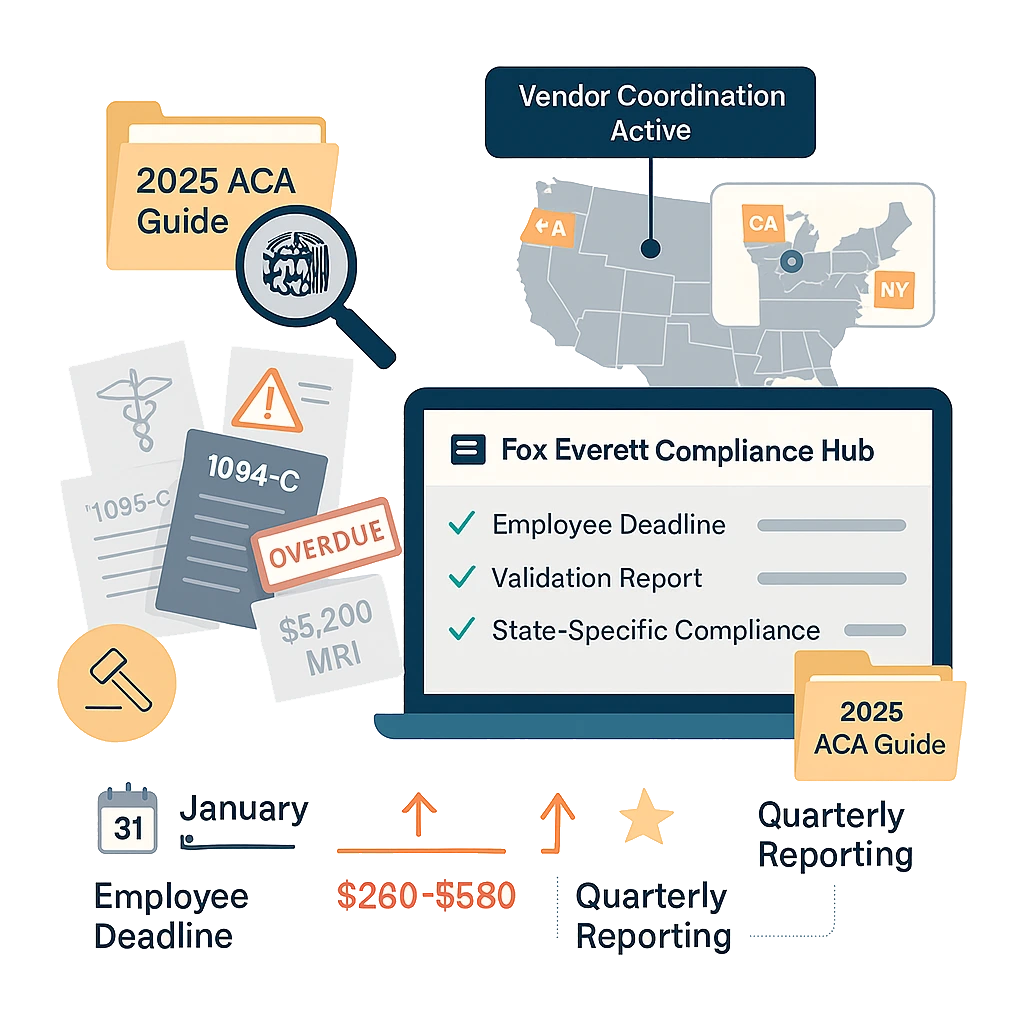
Updated Deadlines and Forms Create New Pressure Points
The IRS has streamlined ACA reporting timelines, but these changes demand immediate attention from HR teams managing compliance.
Form 1095-C Distribution Accelerated
Employee distribution deadlines moved earlier. Forms 1095-C must reach employees by January 31st instead of March 31st. This compression eliminates the buffer period most employers relied on for data verification and correction.
Late distributions trigger $280 per employee penalties. Fora 200-employee company, missing this deadline costs $56, 000 minimum.
Electronic Filing Thresholds Lowered
The IRS reduced electronic filing requirements from 250 to 100 forms. More employers must now navigate electronic submission systems, creating new compliance burdens for mid-market companies.
Paper filing penalties increased to $580 per form for companies exceeding thresholds. Manual processes that worked in 2024 become expensive mistakes in 2025.
Form Updates Require System Changes
Forms 1094-C and 1095-C include new data fields tracking healthcare affordability calculations. Payroll systems need updates to capture required information accurately.
Missing or incorrect data in these fields creates presumptions of violations during IRS examinations.
State-Specific Requirements Emerge as Compliance Wildcards
States are layering additional mandates onto federal ACA requirements, creating complex compliance matrices for multi-state employers.
California Expands Reporting Scope
California now requires detailed reporting on all health plan offerings, not just minimum essential coverage. Employers must document wellness programs, HSA contributions, and voluntary benefits.
The state cross-references federal filings with California submissions. Discrepancies trigger automatic audits with penalties starting at $5,000 per violation.
New York Implements Real-Time Tracking
New York mandates quarterly reporting for employers with 50+ employees. The state monitors coverage gaps and affordability failures throughout the year rather than waiting for annual filings.
Employers missing quarterly deadlines face immediate penalties and mandatory corrective action programs costing $25,000 annually.
Multi-State Complexity Multiplies
Companies operating across state lines face conflicting requirements. What satisfies federal compliance may violate state mandates, forcing employers to maintain multiple reporting systems.
What the IRS Focuses on Now
IRS enforcement has shifted from broad compliance sweeps to targeted examinations of specific violation patterns.
Affordability Safe Harbor Abuse
The IRS scrutinizes employers claiming affordability safeharbors without proper documentation. Common violations include:
- Using incorrect poverty line calculations
- Applying safe harbors to wrong employee categories
- Missing required notifications to employees
- Inadequate record-keeping supporting safe harbor elections
Violations carry $4,460 per employee penalties plus potential shared responsibility payments.
Variable Hour Employee Classification
The IRS examines how employers track and classify variable hour workers. Mistakes in measurement periods or stability determinations create expensive violations.
Incorrect classifications trigger both ACA penalties and potential wage and hour violations, compounding legal exposure significantly.
Third-Party Reporting Coordination
Many employers struggle coordinating ACA reporting between payroll vendors, benefits administrators, and internal systems. The IRS finds discrepancies through automated matching programs.
Inconsistent reporting creates penalties even when coverage was actually provided, making vendor coordination essential for compliance.
How to Avoid Common Filing Mistakes
These preventable errors cost employers millions annually in unnecessary penalties and legal fees.
Data Validation Before Submission
Implement systematic data reviews before filing deadlines. Common errors include:
- Mismatched employee identification numbers
- Incorrect coverage codes for family members
- Wrong affordability calculations
- Missing dependent information
Missing documentation creates presumptions of violations during examinations, shifting burden of proof to employers.
Vendor Coordination Protocols
Establish clear communication channels with all ACA reporting vendors. Define data exchange schedules, validation procedures, and error correction processes before problems emerge.
Many penalties result from vendors missing deadlines or submitting incorrect data, but employers remain legally responsible for compliance failures.
Fox Everett's ACA Support Services Keep You Compliant
Our boutique approach means dedicated expertise managing your ACA compliance while you focus on running your business.
Proactive Compliance Management
We track all filing deadlines, form updates, and regulatory changes affecting your company. Our team handles data validation, form preparation, and submission coordination to ensure timely, accurate filings.
Monthly compliance reviews identify potential issues before they become penalties, protecting your company from costly violations.
Multi-State Expertise
Our specialists understand the complex interaction between federal ACA requirements and state-specific mandates. We maintain compliance matrices for all jurisdictions, ensuring your company meets every applicable requirement.
Vendor Integration Services
We coordinate with your existing payroll and benefits vendors to streamline ACA reporting. Our systems integrate seamlessly with major platforms, eliminating data transfer errors and submission delays.
When problems arise, our team provides immediate response and correction services, minimizing penalties and regulatory exposure.
Simplify Your 2025 ACA Compliance
ACA compliance gets more complex every year, but with the right preparation, you can avoid penalties and regulatory headaches. Fox Everett offers detailed strategies, deadline calendars, and best practices to keep your company compliant. Contact Fox Everett today to book a discovery call and learn why mid-market employers trust our boutique expertise for ACA compliance protection.


